Can You Get an STI Without Having Sex?
In the realm of sexual health, there’s a prevailing misconception that Sexually Transmitted Infections (STIs) solely accompany sexual activities. However, the reality extends beyond the sheets, with instances of STIs being transmitted without engaging in intercourse. Hope Across The Globe aims to dispel myths and promote a comprehensive understanding of STIs. In this exploration, we’ll navigate the various avenues through which one can contract an STI without having sex, emphasizing the significance of recognizing non-sexual transmission routes. For those seeking clarity on their sexual health, we offer reliable and confidential STD testing in Jacksonville, FL, and beyond, ensuring accessible and comprehensive healthcare services for everyone.
1. Demystifying Non-Sexual Transmission
Contrary to widespread belief, STIs aren’t exclusively linked to sexual contact. While sexual activities undoubtedly contribute to transmission, acknowledging non-sexual routes is imperative for a holistic understanding. It’s crucial to comprehend these alternative transmission routes, paving the way for destigmatization and a more informed approach to sexual health.
– STIs and Non-Sexual Transmission
The conventional narrative surrounding sexually transmitted infections (STIs) has often been centered around sexual activities as the primary mode of transmission. However, we urge a shift in perspective and highlight that STIs can be contracted through avenues other than sexual encounters. This understanding is critical for public health awareness as it recognizes the diverse ways in which individuals may be exposed to and contract STIs. From mother-to-child transmission during childbirth to sharing needles or engaging in non-sexual close contact, acknowledging these non-sexual transmission routes is essential for developing comprehensive sexual health strategies.
Incorporating these considerations into sexual health discussions not only broadens the scope of preventive measures but also emphasizes the need for inclusive education. It encourages healthcare professionals, educators, and individuals to recognize the full spectrum of transmission possibilities, fostering a more informed and empowered approach to sexual health.
– Breaking Down Stigma through Awareness
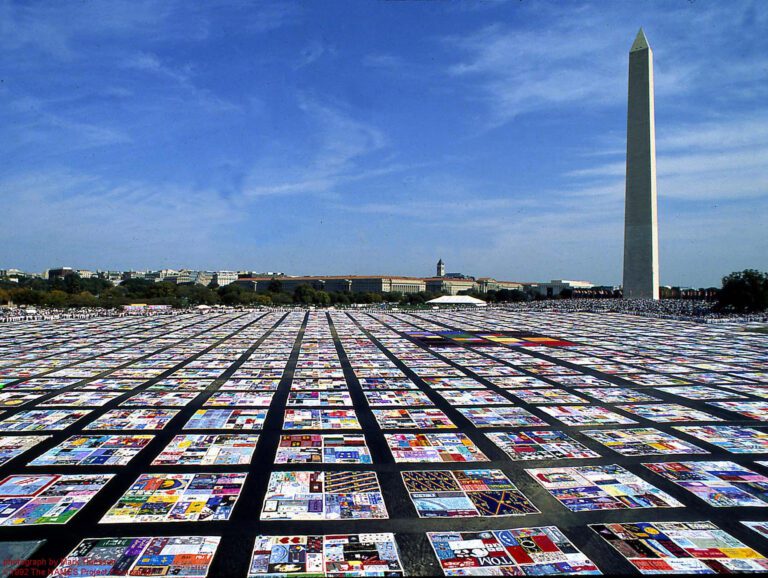
The stigma surrounding STIs can lead to harmful consequences, such as discrimination, social isolation, and delayed or inadequate medical care. To counteract this, we emphasize the role of increased awareness in breaking down stigma. By spotlighting non-sexual transmission routes, it challenges preconceived notions and dispels myths, paving the way for a more open and understanding mindset.
In practical terms, this means integrating comprehensive sexual health education into schools, healthcare settings, and community programs. By providing accurate information about the various ways STIs can be transmitted, society can work towards reducing the judgment and discrimination associated with these infections. Creating platforms for open dialogue and destigmatizing conversations around sexual health ensures that individuals feel more comfortable seeking information, testing, and treatment, ultimately contributing to a healthier and more supportive community.
– Holistic Approach to Sexual Health
A holistic approach to sexual health goes beyond traditional perspectives that solely focus on sexual activities. This passage advocates for considering various transmission avenues, including non-sexual ones, to promote a more comprehensive view of sexual health. Understanding that STIs can be transmitted through means such as sharing needles, from mother to child during childbirth, or even through non-sexual close contact prompts a reevaluation of preventive measures and risk assessments.
To adopt a holistic perspective, education is key. Schools, healthcare providers, and public health campaigns should incorporate information about all potential transmission routes, fostering a culture of informed decision-making. This not only encourages individuals to take responsibility for their sexual health but also promotes a broader societal understanding that contributes to the overall well-being of communities. A holistic approach encourages a proactive stance towards sexual health that encompasses prevention, testing, treatment, and destigmatization efforts, creating a more resilient and informed society.
2. Maternal Connections: STIs and Mother-to-Child Transmission
Among the prominent non-sexual transmission routes is from an infected mother to her child during pregnancy, childbirth, or breastfeeding. The role of prenatal care, antiretroviral therapy, and informed decision-making for expectant mothers in averting mother-to-child transmission cannot be overstated.
– Pregnancy and STIs
The exploration of the intersection between pregnancy and sexually transmitted infections (STIs) underscores the nuanced challenges that expectant mothers may face. We not only acknowledge the potential risks of STI transmission during pregnancy but also emphasize the pivotal role of prenatal care in mitigating these risks. Beyond prenatal care, it is crucial to understand the specific nuances of STI risks and the importance of early detection and intervention. A proactive approach to maternal health that incorporates STI screening as an integral component of comprehensive prenatal care shouldn’t be underscored.
Highlighting the relationship between STIs and pregnancy encourages healthcare providers to incorporate routine STI testing into prenatal care protocols. This approach ensures that potential infections are identified early, allowing for timely intervention and management. By fostering a deeper understanding of the interconnected nature of pregnancy and STIs, we contribute to a more informed and empowered maternal healthcare landscape.
– Childbirth and STI Risks
We recognize the potential challenges and emphasize measures, such as antiretroviral therapy, that can be taken to prevent mother-to-child transmission during this critical period. Informed decision-making by expectant mothers is a key element in navigating the complexities of STI risks during childbirth.
Empowering expectant mothers with knowledge is crucial for ensuring optimal outcomes. By understanding the potential risks and available preventive measures, mothers can actively participate in decision-making processes related to their childbirth experiences. A collaborative approach between healthcare providers and expectant mothers, fostering a sense of shared responsibility for maternal and child health is crucial at this stage.
– Breastfeeding Considerations
It is crucial to understand how certain STIs can be transmitted through breast milk and, even more so, to be informed of the preventive measures that can be taken to protect the child. This nuanced discussion encourages a balanced perspective that considers both the nutritional benefits of breastfeeding and the potential risks associated with STI transmission.
The importance of a supportive healthcare environment that guides mothers through the complexities of balancing the nutritional advantages of breastfeeding with the need to prevent STI transmission cannot be overemphasized. This approach acknowledges the multifaceted nature of maternal health and child health, contributing to a more holistic understanding of the factors at play during the postpartum period.
3. The Blood Bond: Intravenous Drug Use and STIs
For individuals involved in intravenous drug use, sharing needles amplifies the risk of bloodborne transmission of STIs. This section explores the complexities of this mode of communication, discussing harm reduction strategies, the importance of sterile needle use, and the role of community support in addressing the root causes of drug-related STIs.
– Needle Sharing Risks
There are profound risks associated with sharing needles among individuals who engage in intravenous drug use. It goes beyond a surface-level examination, emphasizing the heightened vulnerability to bloodborne sexually transmitted infections (STIs) within this population.
Acknowledging the risks associated with needle sharing serves as a critical step in public health discourse. By drawing attention to the specific vulnerabilities of this demographic, it lays the foundation for targeted interventions that address the unique challenges posed by intravenous drug use. This comprehensive understanding is essential for developing effective strategies to mitigate the transmission of STIs within this high-risk population.
– Harm Reduction Strategies
The promotion of sterile needle use is a cornerstone of harm reduction efforts. By emphasizing the importance of providing access to clean needles, it underscores the potential impact of such initiatives on reducing the spread of bloodborne STIs among individuals engaged in intravenous drug use.
Community-based harm reduction strategies are explored as powerful tools that can actively contribute to minimizing the risk of STIs. This includes education on safe practices, the distribution of sterile needles, and the creation of safe spaces where individuals can access resources and support without fear of judgment. By promoting harm reduction, we advocate for a compassionate and pragmatic approach that recognizes the complex challenges faced by those involved in intravenous drug use.
– Community Support for Drug Users
Beyond immediate interventions, we have to explore the broader perspective of addressing the root causes of drug-related STIs. By recognizing the multifaceted challenges faced by individuals in this context, we advocate for a holistic approach that extends beyond the realm of healthcare.
Community support is positioned as a key element in providing a safety net for those navigating the complexities of intravenous drug use, understanding and addressing the underlying factors contributing to drug-related STIs that can positively impact both individuals and communities. This may involve mental health support, access to rehabilitation services, and initiatives aimed at reducing systemic issues that contribute to drug-related health disparities. By fostering a sense of community, we advocate for a compassionate and inclusive approach that goes beyond medical interventions, recognizing the interconnected nature of health and societal well-being.
4. Skin-to-Skin Contact: STIs Beyond Intercourse
Certain STIs, such as herpes and HPV, can be transmitted through skin-to-skin contact. This section explores the nuances of these infections, discussing preventive measures, the importance of regular screening, and the role of vaccination in reducing the risk of skin-to-skin-transmitted STIs.
– Herpes and Skin Contact
It is also vital to delve into the intricacies of sexually transmitted infections (STIs), particularly focusing on herpes and its transmission through skin-to-skin contact; moving beyond conventional discussions centered on sexual intercourse to shed light on the specific characteristics of infections like herpes. By emphasizing the potential transmission through skin contact, traditional perceptions of STI risks are challenged, advocating for a more nuanced understanding of transmission routes.
Exploring the dynamics of herpes transmission highlights the importance of education in sexual health. Understanding that skin contact can be a mode of transmission prompts individuals to adopt preventive measures beyond those typically associated with sexual activities. This knowledge contributes to a more informed and empowered approach to sexual health, encouraging individuals to engage in open conversations with healthcare providers about their risks and prevention options.
– HPV and Non-Sexual Transmission
Shifting the focus to Human Papillomavirus (HPV), the potential for its transmission through non-sexual means must be explored. The discussion must extend beyond sexual intercourse, specifically around HPV risks, as well as preventive measures such as vaccination and other effective strategies for reducing the risk of skin-to-skin-transmitted STIs.
Exploring HPV’s non-sexual transmission routes underscores the importance of a comprehensive approach to sexual health education. Highlighting vaccination as a preventive measure not only offers valuable information to individuals but also advocates for the incorporation of vaccination discussions into broader public health initiatives. We encourage individuals to proactively engage with healthcare professionals to explore vaccination options and consider them integral components of their overall sexual health strategy.
– Vaccination for STI Prevention
The importance of considering vaccination as part of a comprehensive strategy for sexual health is vital. Individuals should view vaccination not only as a protective measure for themselves but also as a contribution to community-wide efforts to reduce the prevalence of specific STIs.
Positioning vaccination as a key component of STI prevention challenges any existing hesitations or misconceptions individuals may have about vaccines. It fosters a culture of preventive healthcare, urging individuals to be proactive in safeguarding their well-being. This shift in perspective advocates for a collective responsibility towards public health, promoting vaccination as a powerful tool to protect oneself and contribute to the broader goal of reducing the incidence of preventable STIs within communities.
5. Environmental Factors: Public Spaces and STI Transmission
Surprisingly, certain STIs can be contracted through environmental factors and public spaces such as shared rooms. The importance of personal hygiene, awareness, and community efforts in minimizing these risks cannot be overemphasized.
– Environmental Transmission
Exploring the possibility of contracting certain infections through environmental factors and public spaces is also vital to redefining the scope of sexual health discussions and encouraging individuals to consider a broader spectrum of preventive measures; challenging conventional perceptions and emphasizing the need for heightened awareness about potential risks that extend beyond intimate encounters.
Understanding that STIs can be contracted in shared environments introduces a new layer of complexity to the public health discourse. It calls for innovative approaches to education and awareness campaigns that equip individuals with the knowledge needed to navigate these unconventional risks. By acknowledging environmental transmission, we promote a proactive stance, urging communities to collectively address and mitigate potential threats in communal spaces.
– Public Spaces and STI Risks
Building upon the concept of environmental transmission, the risks associated with non-sexual transmission in public spaces must be explored, understanding how infections can be contracted beyond intimate settings and the role that personal hygiene practices play in reducing the likelihood of acquiring STIs in communal areas.
This encourages a paradigm shift in how individuals perceive their interactions with public spaces. It underscores the significance of informed decision-making in daily activities, urging people to be mindful of potential risks and take proactive measures to protect their sexual health. By focusing on non-sexual transmission dynamics in public spaces, we advocate for a holistic understanding of STI risks that go beyond traditional boundaries.
– Hygiene Practices for STI Prevention
Adopting certain habits contributes not only to individual sexual health but also to the overall well-being of communities in various environments. Encouraging individuals to prioritize personal hygiene practices becomes a call to action for fostering a culture of health-conscious behaviors. This extends beyond the individual level to encompass a communal responsibility for maintaining clean and safe environments. Individuals must take charge of their own health while contributing to the collective effort to minimize the risk of STIs in shared spaces. By highlighting the significance of hygiene practices, we advocate for a comprehensive approach to sexual health that considers both personal choices and their broader implications for public well-being.
6. The Impact of Non-Sexual Transmission on Public Health
Understanding non-sexual transmission routes is not only crucial for individual health but also for public health. The need for comprehensive sex education, accessible healthcare services, and destigmatization efforts to create a more informed and supportive society cannot be overemphasized.
– Community Health Implications
The profound ripple effect of understanding non-sexual transmission routes goes beyond individual health considerations; further, it contributes to the broader landscape of public well-being. Recognizing the community health implications of STIs challenges societies to prioritize not only individual health but also the creation of environments that support the well-being of all members. This understanding serves as a catalyst for collaborative efforts, encouraging communities to address STIs comprehensively and implement strategies that promote a collective culture of health and responsibility.
– Importance of Comprehensive Sex Education
The pivotal role of comprehensive sex education in shaping a more informed and empathetic society is of equal importance. We advocate for initiatives that go beyond basic information, delving into the complexities of STIs and transmission routes. Comprehensive sex education becomes a cornerstone of building a society that is not only knowledgeable about sexual health but also compassionate in its attitudes. Educational institutions and communities are encouraged to embrace a comprehensive approach that equips individuals with the tools to navigate the complexities of sexual health responsibly. By fostering an informed society, comprehensive sex education becomes a powerful tool for destigmatizing conversations around STIs and promoting a culture of openness and support.
– Breaking Down Stigma in Public Health Initiatives
By acknowledging the power of collective action, communities are urged to actively engage in destigmatization campaigns that foster understanding and acceptance. Public health initiatives play a pivotal role in shaping societal norms and attitudes. Organizations, healthcare providers, and community leaders are encouraged to collaborate on destigmatization efforts, making it clear that breaking down barriers surrounding STIs is a shared responsibility. By emphasizing the importance of empathy and support, we advocate for the creation of inclusive spaces where individuals affected by STIs can access resources, receive non-judgmental care, and contribute to a society that values the well-being of every member.
Conclusion
Recognizing non-sexual transmission routes of STIs is vital for fostering a more comprehensive understanding of sexual health. At Hope Across The Globe, we advocate for education, awareness, and accessible healthcare to empower individuals and communities in the face of STIs. By unraveling the complexities beyond sexual intercourse, we contribute to breaking down stigma and creating a more informed and compassionate society.
Related Tag: STD Testing in Jacksonville FL